Image credit: Mariah Aro Sharp @mightymooseart
Rav’s Repro is a column in which Erin explores all topics related to reproduction and reproductive rights.
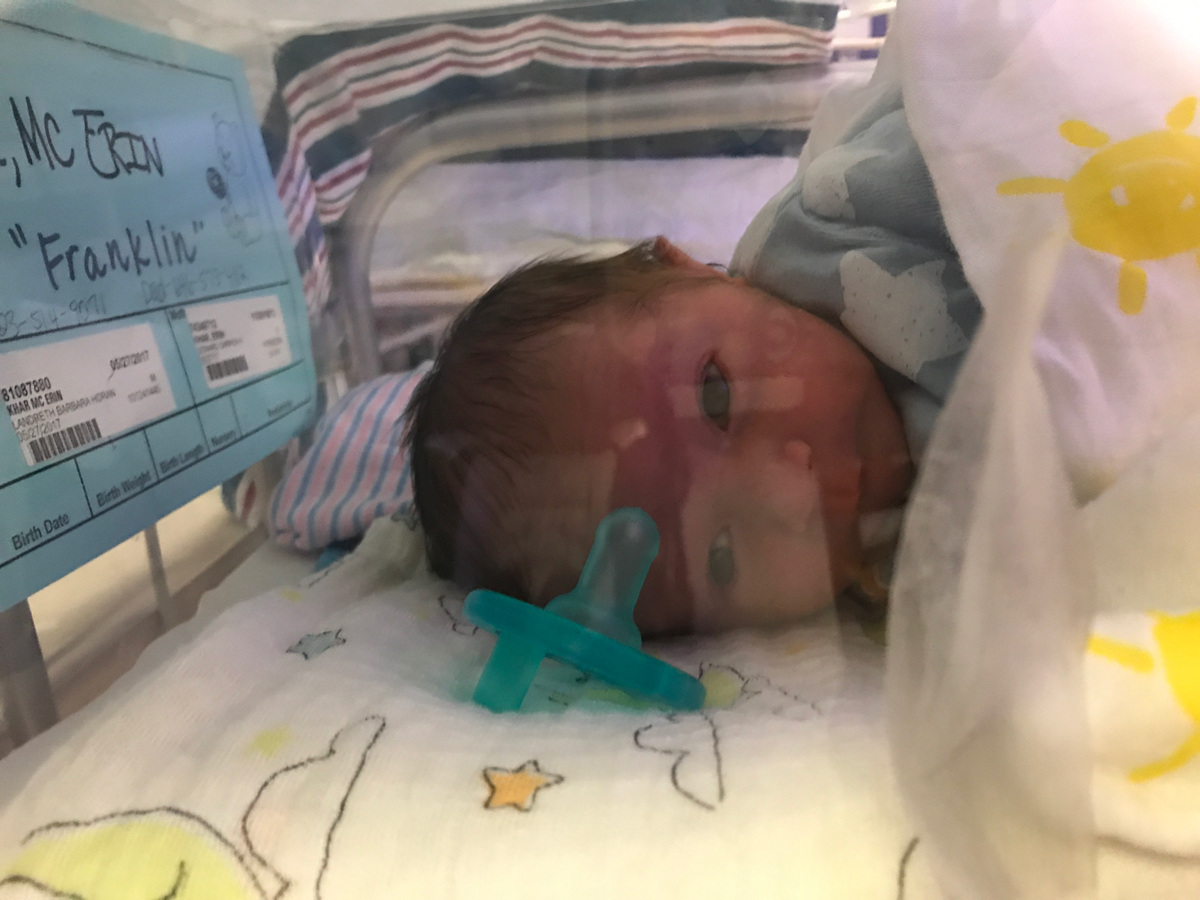
My water broke at exactly midnight. I was 34 weeks and four days pregnant. The birth itself was relatively smooth. But, because I was less than 35 weeks, I knew he would have to be taken to the NICU unit for at least a couple of days. Okay, I thought, standard procedure… No big deal.
Before May 27th of this year, I thought I understood what the NICU was like. I had spent time in one in Los Angeles, some years ago, when one of my best friends gave birth to premature twins. I thought I knew what to expect. I was wrong.
Because when it’s your baby in the NICU, when you’re there day after day, and you have no control over ANYTHING, it’s nothing like what you expected. It’s nothing like what you thought you knew.
September is NICU awareness month. There are so many things I wish I would have known going into those four weeks. I am not a doctor, but I’m sharing them here. If you ever find yourself in that position of being a parent with a newborn in the NICU, this is what I want to tell you…
The sounds will be nerve-wracking, and then one day you will get used to them.
A few hours after giving birth, I went down to the NICU for the first time. The first thing I noticed, even before I laid eyes on my five-pound baby boy with so many wires and tubes connected to him, was the cacophony of sounds — beeps, dings, alarms, and repeat.

The first room Franklin was in was for new admits and some babies who had been there awhile but needed the most critical level of care. All of them were connected to monitors, most of them on respiratory assistance.
I would come to know the codes for the various alarms — bradycardia, tachycardia, low RR (respiration rate), high RR, low Oxygen saturation. And there were more. And with tiny babies who are just hours or days old, their systems are not regulating so well, so these alarms go off constantly.
At first, I would jump every time I heard one, and I would look to Franklin’s monitor to see if it was him or a baby at Monitor H or Monitor C. The nurses rarely jumped when these alarms went off and I came to learn over time that the different alarms indicate a different level of urgency and that mostly, they should just be tuned out.
Don’t go to rounds.
After the first day in the NICU, the nurses told me that I could come to rounds in the morning so that I could get the report from the team of NICU doctors. This sounded like a good idea. And so, the day after he was born, I went to rounds. Alone. Because my husband was at home with Atticus, my older son.
What I didn’t know was that he had a rough night, that he wasn’t able to regulate the pressure in his tiny lungs. As I listened to the team talk as if I were not there, my body swelled with tears that I was trying to hold in.
I heard that he would be taken off the CPAP, intubated, and put on a respirator. I heard that the term for what was happening to him was Persistent Pulmonary Hypertension. I heard they were going to give him morphine because he was agitated. I heard they would be doing an echocardiogram of his heart to rule out a heart defect, and a scan of his head to make sure there was no bleeding in his brain.
When they were done, the lead doctor turned to me and asked me if I had any questions, but I couldn't get the right words out because I was choking on all the tears I had been desperate to contain.
“But, he’s going to be okay, right? I’m freaking out. Should I be freaking out?”
“This is within the normal range of what we see in premature infants.”
WTF does that mean?
Because I’m a masochist, I went to rounds again the following day and had a similar experience. After rounds, one of the NICU nurses explained things to me (in a language my overly tired, hyper-emotional brain could process). And she told me that I didn’t have to go to rounds, that I can always get the information after rounds from one of the nurses or one of the doctors. Which leads me to the next important thing I learned…
The nurses will save your sanity.
Those women (and one man) are angels. No, literally, they are angels. They were the ones taking care of my baby, minute by minute. They were the ones who held my hand, who told me it was going to be okay, who promised me I would be taking my baby boy home.

They were the ones who held me when I cried, who gave me the maternal support I so desperately needed. They were the ones who explained things, who reminded me to eat and drink water. And they were the ones who told me to go home because I had to get some sleep.
You need sleep.
Perhaps the most painful part of the NICU is the time each day when you leave to go home. I think I cried every single time. And sometimes, I came back later.
This became especially challenging as he was taken off the breathing apparatus and was able to start nursing. All I wanted was to feel that baby breathing against my skin. I wanted to feed him and comfort him at all times.
But, that’s not possible. You have to get some sleep. You will be a better parent to your little one if your brain has had a chance to rest. And you can trust that the care babies get in a NICU is superb.

The information will change so quickly.
This is particularly the case in the first few days. By the time I had relayed information to my husband, or our parents, or my friends, it would change again.
I learned that updating people more than once a day (if that) was pointless and an exercise in futility. Which leads me to…
You need a point person to update everyone, or you will end up wanting to throw your phone out the window.
As I mentioned, that information will be changing… A LOT. And when you update people, they will likely have questions, questions you will probably not have the answers for.
By day two, I wanted to pull my hair out. I made a group text for our immediate family and let them know that I would update them once a day when I had pertinent information.
What I should have done is asked one person to disseminate the information and field questions. But, the once-a-day plan did work out fairly well.
It will likely be two steps forward and one step back.
This is what the nursing team told me, repeatedly. And they were right.
The NICU is like no other field of medicine. The way premature infants are treated is different than how an adult, a child, or a two-month-old baby would be treated.
The framework in the NICU is basically: Let's see if the baby is ready to do this… Nope, let’s give them some more support… Oh, now they’re moving fast… Oh, they need a little more time.
Franklin’s discharge date changed four, maybe five times. And that was painful. I was in a constant state of working on acceptance. And, each time, I would get there, but it was not easy.
Chances are, your little one will come home, and those days or weeks or months in the NICU will become but a moment in time.
This is also something those nurses told me. I knew in my heart that they were right, but it was hard to remember this from one day to the next. I never anticipated that he would be there for one day shy of four weeks. But he was.
The nurses also told me that the babies decide when they are ready to go home. The babies let us know, by being able to breathe and regulate their heart rate and eat and keep their temperature steady.

Although those days in the NICU that seemed never-ending are still fresh for me, they were right: As these weeks — and now months — since the NICU have passed, the time spent there does feel more and more like a moment in time.
We are so lucky. Because baby Franklin came home. I know our experience was nothing compared to what some families go through there — when they really don’t know if they will bring their baby home.
What I want to say is this:
To the doctors and nurses and techs of New York-Presbyterian Hospital (and elsewhere) who work to save our babies, I cannot thank you enough. You are miracle workers.
To the families with little ones in the NICU, my heart goes out to you. I know how hard it is to leave at the end of every day. I know how frustrating it is to accept that there is little you can do, but be there. I am well-acquainted with the fear and desperation. I send you my love. And I hope, and I have faith, that you will bring your baby home, and that the time in the NICU will become just a moment in time.

You Might Also Like:
Rav's Repro: The Birth Of Our Rainbow Baby
Can We Stop Judging Other People's Reproductive Choices?
Rav's Repro: Failure To Thrive